Toddler sleep – aka, a whole new ballgame. If you’ve made it through the baby sleep stage relatively unscathed, hitting the toddler sleep stage can be a huge eyeopener. Sleep issues at this age can be formed so quickly, as with toddlers, you give an inch, they take a mile. There are so many more ways of resisting change, resisting sleep, and boundary/limit testing starts to impact sleep in a major way. The good news is that if you are prepared for it to happen, we can still make it through these years unscathed, and this blog post series is meant to give you the preparation you need!
I’m breaking down the things to look out for by age – sleep needs/schedule at each age, potential issues, and potential changes. I would recommend reading through each age even if you don’t have a child at that age as issues/changes can really occur at any time, and we want to be fully prepared for anything! I am starting with the 1-year-old crowd. I had originally planned for all ages to be included on the same blog post, but as per usual I was far too wordy so I will be breaking this down year by year [so make sure you come back for age 2, 3, and 4!]
I hope you find this post helpful and if you do, please share it with your friends and family!
1 YEAR OLD SLEEP: the last of the regressions
Sleep needs
12-14 months: average 13.5-13.75 hours (low 13 hours, high 14.25 hours)
15-18 months: average 13-13.5 hours (low 12.5 hours, high 14 hours)
19-23 months: average 12-12.5 hours (low 11.5 hours, high 13 hours)
Schedule
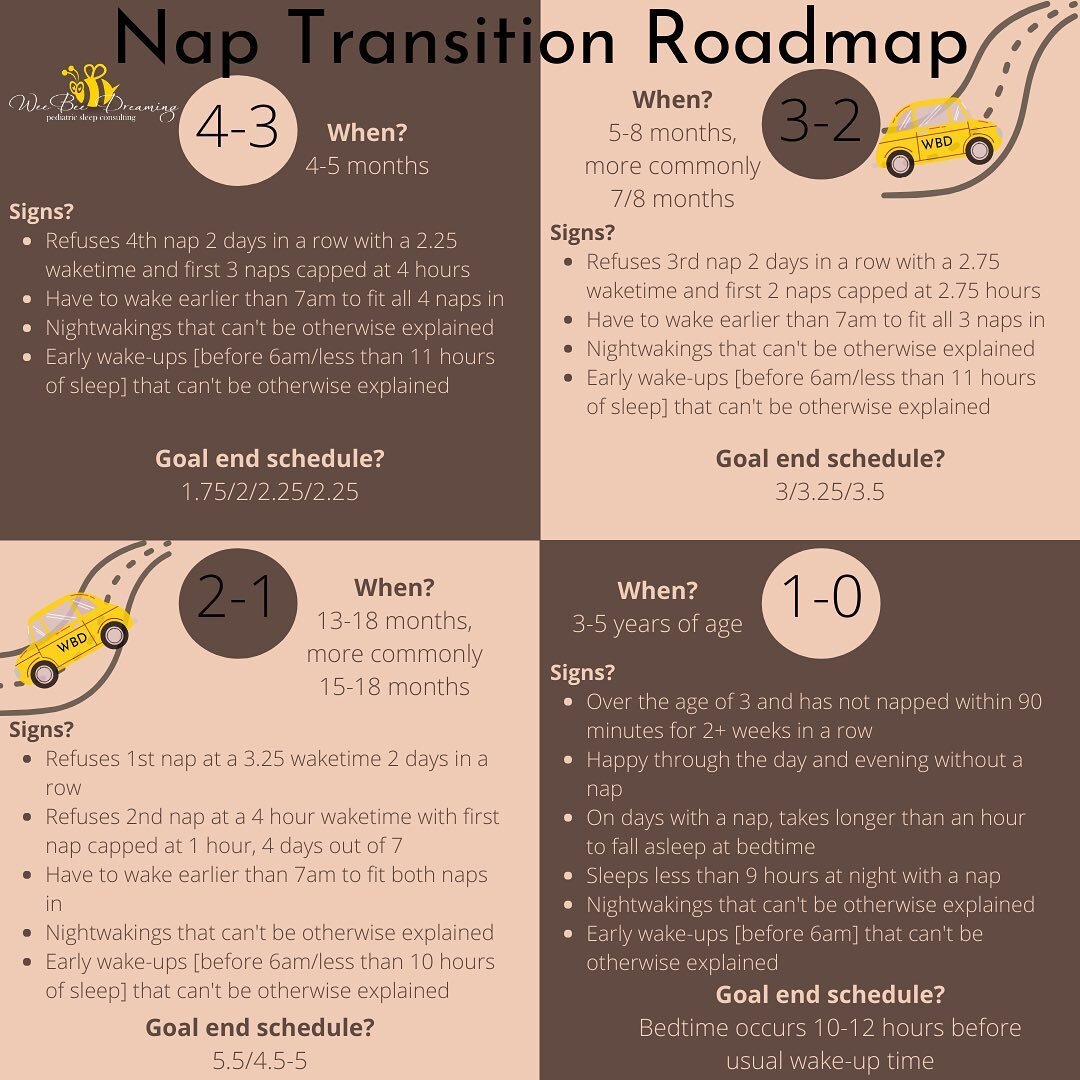
At this age, our main goal is preserving a 2-nap schedule for as long as feasibly possible. Why? The awake time needed to sustain 1 nap is much longer than on a 2-nap schedule, and if your toddler isn’t ready for the jump, a sleep debt can accumulate that results in short naps, nightwakings, early wakeups, and crummy sleep in general. The typical age to transition to 1 nap is between 13-18 months, more commonly 15-18 months, but the closer to 18 months that you can get, the better. If you’ve hit 18 months and you’re still on 2 naps, I would recommend starting the transition at that point, as once sleep needs decrease around 19 months, the transition can actually be more challenging.
If you’ve tried it all to hold onto that 2nd nap and it’s just not happening or if you have to transition your child to 1 nap due to schedule constraints [aka starting daycare], then make sure you give yourself enough time to make this a gradual transition. I recommend transitioning over the course of a 4-week period, so if you know you need your toddler on 1 nap, begin the transition a month prior. Check out my Comprehensive Nap Transition Guide for a step-by-step/day-by-day transition plan for every singe nap transition!
The schedules below will give you an overview of what this transition should look like.
The most important takeaways are:
The transition should be gradual
Use a 2nd nap/quiet time when the 1st nap ends before noon
Don’t be afraid of an earlier bedtime during the transition
Your end schedule should have the nap starting no earlier than 12:30pm [down no earlier than 12:15pm] to avoid a) a perpetual early bedtime or b) a long stretch before bedtime, neither of which are ideal!
Prior to the transition [age 13-18 months]:
6:30am - up for the day
7:00am - breakfast
9:00am - snack
9:45am - 10:45am - nap#1 [to hold off the transition until this point, it's beneficial to cap this nap at 1 hour]
12:00pm - lunch
2:00pm - snack
2:45pm - 3:45pm - nap#2 [a full 4 hours of awake time between naps 1 and 2]
5:30pm - dinner
6:30pm - bedtime routine [should not include any milk, last milk with dinner!]
7:15pm - bedtime [asleep by this time]
One week into the transition:
6:30am - up for the day
7:00am - breakfast
9:30am - either a big snack OR lunch split in half
10:15am - 12:15pm - nap [we pushed out the first nap by 15 minutes every 3 days. If the nap ends at noon or later, we move to bedtime. If the nap ends before noon, we do a catnap/quiet time around 3:00pm]
12:30pm - either a big snack OR the other half of lunch
2:30pm - small snack
5:00pm - dinner
5:30pm - bedtime routine
6:15pm - bedtime
Two weeks into the transition:
6:30am - up for the day
7:00am - breakfast
10:00am - either a big snack OR lunch split in half
11:00am - 1:00pm - nap [we continued to push the nap out by 15 minutes every 3 days]
1:15pm - either a big snack OR the other half of lunch
3:15pm - small snack
5:30pm - dinner
6:00pm - bedtime routine
6:45pm - bedtime
Four+ weeks into the transition [transition complete]:
6:30am - up for the day
7:00am - breakfast
9:00am - snack
11:30am - lunch
12:30pm - 2:30pm - nap [nap was pushed out by 15 minutes every 3 days to a 5.5 hour waketime but with no put down before 12:15pm]
3:00pm - snack
5:45pm - dinner
6:15pm - bedtime routine
7:00-7:30pm - bedtime
At the end of the transition, we are looking for the nap to occur 5.5+ hours after wakeup time [wakeup time should be no later than 8:00am], the nap should be between 1.5-3 hours in duration and it should end no later than 3:00/3:30pm to preserve a bedtime of 8:00pm or earlier [to ensure sufficient nighttime sleep]. The bedtime waketime should be between 4.5-5 hours and this schedule stays strong until age 2 [although you may need to play around with nap duration before then, and start capping the nap closer to 2.5 hours or possibly even 2 hours if you are noticing a longer nap interfering with nighttime sleep, especially at 19+ months when sleep needs typically decrease].
Common changes
Pacifier
There are a lot of different opinions on when is the best time to eliminate the pacifier. My opinion? Somewhere between 16 weeks and 6 months. Why? Out of sight is out of mind at that age and the pacifier is usually small beans to get rid of [and then you avoid months of the paci dance too!]
The next elimination age that I would keep in mind to make things easier on everyone, is weaning from it before you hit 18 months. After 18 months, the pacifier becomes much more like a security blanket to your child, and trying to take away a toddler’s security blanket, as you can imagine, is not usually a fun time!
The next elimination age that I would keep in mind is while you have containment on your side [aka before you move to a bed]. I’m sure you can see why that would be easier! Also, the closer you get to age 2.5-3, the more likely it is that when the pacifier goes, the nap goes with it [noooo!]
If you’ve hit age 1 and you have decided now is the time to ditch the pacifier, you may be wondering what the best way of doing that might be. Well truth be told, there aren’t many ways of talking your child into this change, so taking more ‘cold turkey’ strategy is usually the most realistic option.
Step 1: make the pacifier only available at sleep times.
Step 2: introduce a different security object [if you haven’t already]. A special lovey, stuffed animal, blanket – it can be anything! Work on them attaching to the security object in advance, although they may not form a super strong attachment to it until the current lovey [aka the pacifier!] is out of the mix.
Step 3: talk to your child about these changes [they understand more than you think!] Have a countdown of a few days before you plan to wean. Consider using a fun story about where the pacifier is going. Is the pacifier fairy scooping them up to deliver to babies that don’t have any? And maybe replacing with a gift? Do you plant them in a garden and lollipops grow where the pacifiers were? Do you sew them into a special stuffed animal? The internet is your friend here for cute ideas! Other options include ‘losing’ the pacifiers slowly over the course of a week or having your dentist talk to your child about needing to get rid of the pacifier for oral health reasons. You know your child best here!
Step 4: bye-bye pacifier! It’s important that the first time your child sleeps without the pacifier is at bedtime [when the drive to sleep is higher and it’s much easier to fall asleep] and then follow with nap(s) the next day. Choose a sleep training method that you feel comfortable with [find a list here!] and then go for it. It will very likely be easier than you are anticipating, and while every child has a different level of adaptability, if you are consistent, it can be forgotten about within a week. I highly recommend that you get rid of ALL the pacifiers [no emergency back-ups!] as this makes it much easier to stay the course, and we owe it to our kids to stay consistent!
Starting daycare
If you live outside of Canada, it is very likely that your child has already started daycare before the age of 1, but if not, somewhere between 12-18 months is a common age that this transition occurs. Being prepared for what this will look like for your child can help ease the transition. What things should we be asking about?
Schedule: if you are starting daycare after 12 months, it is very likely that the daycare will have their own nap schedule that your child will have to adhere to. I have seen a daycare’s nap starting anywhere between 11:00am and 1:30pm, so knowing this in advance will be helpful information. If the nap at daycare is starting earlier than 12:30pm, I would strongly recommend waking your child no later than 7:00am to ensure sufficient awake time before the nap. With an early nap, the downside is that you won’t be able to properly follow the 4.5-5 hour waketime before bedtime that I recommend, because if your child is napping from 11:00am-1:00pm, that means a bedtime of 5:30-6:00pm [not realistic and not recommended!]
So what you’ll want to look at is your child’s total waketime. This is the amount of time your child is awake in a day. There is a minimum/maximum amount of time we are looking for at each age, and this can help you plan bedtime if the timing of your daycare’s nap is less than ideal [aka too early in the day].
Total waketime by age
12-14 months: 10.25-10.5 hours
15-18 months: 10.5-11 hours
19-23 months: 11.5-12 hours
So how do we use this information to determine bedtime?
Let’s say your child is 15 months old and you are waking them at 7:00am for daycare.
Your daycare’s nap is on the early end, let’s say your child is expected to be asleep by 11:30am.
That means your child is awake 4.5 hours before their nap, leaving another 6-6.5 hours of waketime that we need in a day [to total the above 10.5-11 hours].
You would want to add this 6-6.5 hours before bedtime, to ensure sufficient awake time.
Why is sufficient awake time important? If the amount of time your child is awake during the day is too low, they may very well make up for that by…being awake at night!
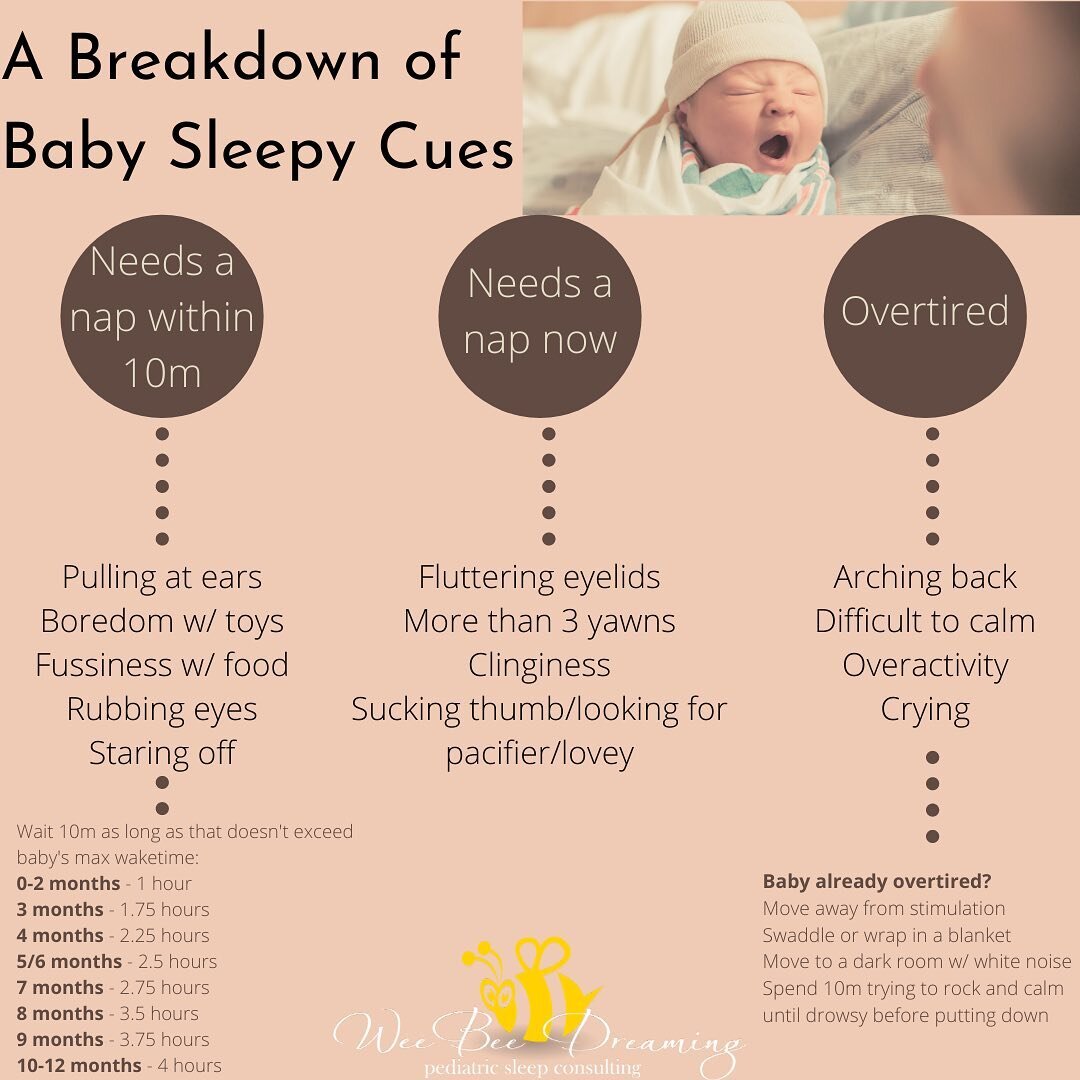
So if your child slept from 11:30am-1:30pm, that means a bedtime between 7:30-8:00pm. With a 2 hour nap, that leaves 11-11.5 hours of sleep needed at nighttime, so a bedtime of 7:30-8:00pm should get you to 6:30-7:00am the next day without issue. Because the awake time before bedtime is longer than recommended, make sure you watch for sleepy cues and consider going on the shorter end of this waketime range, especially if your child is just new to daycare!
I would recommend following your usual schedule on the weekends vs. trying to match daycare’s schedule on weekends!
*If your child is only going to daycare part-time (3 days/week or less) and is under 18 months old and still on 2 naps/day, I would not worry about transitioning them to 1 nap in advance, and I would allow them to continue taking 2 naps/day on home days [aka the majority of days] and simply following the daycare’s 1 nap schedule on daycare days.*
Environment: Just like schedule, the environment is another aspect of daycare that is completely out of our control but good to be aware of in advance! If there are ways we can recreate home for your toddler, it can make the transition to sleeping in an unfamiliar environment a bit easier. Some things to ask would be:
Are you allowed to bring a sleepsack? Or a special blanket/pillow? How about a security object?
Do you use white noise? [many daycares will play music, which is not great but better than nothing!] If not, are you allowed to bring a portable machine?
Do they sleep in cribs or cots? Please note that if the answer is a cot, that does NOT mean you should transition your child to a bed in advance! Please do not do this!
Do they turn off/dim the lights? If they don’t, this also doesn’t mean you should try and introduce light to your child’s sleep environment at home, this will not help. Plus, the peer pressure of other little people sleeping around me is very strong, so even if the environment is less than ideal, this pressure often counteracts that. Keep your stellar home environment!
Once your child has past the ‘acclimation’ stage at daycare [usually about 2 weeks], if their sleep is still poor, asking further questions to investigate can be helpful:
Is someone helping your child to sleep? If this is not something that you do at home, I would be requesting that daycare also gives your child the space to fall asleep on their own at daycare [within reason, as some assistance may be needed if your toddler is being disruptive]. Once your child has acclimated, request that they only intervene when needed, as the downside with someone helping your child to sleep is that they may only end up sleeping for one sleep cycle [30-60 minutes] before waking and being unable to fall back asleep.
Is your child sleeping next to a ‘problematic sleeper’? Some kids can sleep deeply through noises, and others will be more sensitive to this. If your child isn’t napping well, I’d be troubleshooting whether they are in close proximity to another tricky sleeper and if so, perhaps it’s worth requesting they move further away from the action.
Is your child falling asleep easily at nap time or is it taking a while for them to settle? If the latter is the case, especially if it’s coupled with an earlier-than-recommended nap time, you may want to consider waking your child a bit earlier in the morning to build up more sleep pressure before the nap, to hopefully help them settle into sleep more easily and build up enough sleep pressure to take a good nap.
Common issues
The dreaded 18-month regression
The 18-month sleep regression is a developmental phase that typically occurs between 15-24 months, often around 17-19 months. During this period, toddlers can experience significant changes in their sleep patterns, leading to disturbances. This regression often aligns with the transition from two naps to one and coincides with an explosion in cognitive development. Understanding the causes and manifestations of this regression can help you to manage it more effectively.
Why does the 18-month sleep regression occur?
At 18 months, toddlers undergo substantial cognitive development. They start to test limits and explore the world around them more assertively. This developmental leap can disrupt their sleep as they experiment with actions and consequences, such as yelling at bedtime or refusing naps. This period also sees a resurgence of separation anxiety, making bedtime a challenging experience for both toddlers and parents.
The transition from two naps to one nap is a significant milestone that often coincides with the 18-month sleep regression. Rushing this transition or not adjusting bedtime can lead to overtiredness, exacerbating sleep disturbances. Toddlers need a gradual adjustment period to adapt to the new sleep schedule [as per above!]
How does this regression differ from earlier ones?
Unlike earlier regressions (such as the 4-month or 8-month), the 18-month sleep regression is closely tied to significant cognitive developments and the assertion of independence. Earlier regressions are often related to physical growth spurts or the development of new sleep cycles. The 18-month regression is unique in its connection to language development, increased mobility, and the emerging sense of self, making it particularly challenging for both toddlers and parents.
How can you manage this regression?
Setting clear boundaries around sleep times is crucial during the 18-month sleep regression. A consistent bedtime routine helps toddlers understand that it’s time to wind down and go to sleep. Without clear boundaries, bedtime can turn into a prolonged negotiation, leading to increased resistance and sleep issues.
Tips for Setting Clear Boundaries
Consistent Routine: Establish a bedtime routine that includes the same steps in the same order every night. This could involve activities like brushing teeth, reading a book, and singing songs.
Defined End Time: Ensure there is a clear and defined end to the bedtime routine. Use a specific phrase or song to signal that it’s time to sleep.
Avoid Negotiations: Do not negotiate with your toddler during the bedtime routine. Giving in to demands for "one more book" or "one more hug" reinforces stall tactics and undermines the routine.
Toddlers often test limits to assert control over their environment. Providing age-appropriate choices within the bedtime routine can help satisfy their need for control while maintaining necessary boundaries.
Tips for Providing Choices
Offer Options: Let your child choose between two sets of pajamas or two bedtime stories. This gives them a sense of control without compromising the routine.
Assign Bedtime Jobs: Give your child simple tasks like putting toothpaste on the toothbrush or placing their lovey in the crib. This involvement can make them feel more in control and cooperative.
While it can be tempting to resort to quick fixes like letting your child sleep in your bed, these habits can prolong the regression and lead to long-term sleep issues. We never want to resort to long-term habits when dealing with short-term issues.
Tips for Avoiding Bad Habits
Consistent Sleep Routines: Stick to a consistent bedtime routine and avoid introducing new habits that you don’t want to continue in the long term [rocking to sleep, letting your child sleep in your bed, napping in the car/stroller instead of crib, re-introducing sleep crutches like bottles, pacifiers, etc.]
Brief Interactions: Comfort your child as needed but keep interactions brief and boring. Avoid staying in the room or rocking your child to sleep if this isn’t something you are already doing. While it feels like in the moment it will make things easier, in the long-term it won’t!
Separation and Reassurance: Make sure your child sees you leave the room after putting them down. Offer reassurance with a quick verbal check-in over the monitor if needed but maintain consistency in not re-entering the room [or if you do re-enter the room, make sure it’s brief and boring!] The worst way to deal with separation anxiety is to avoid separating. This is like telling their brain, ‘yes separating IS something you should be worried about, because as soon as you began to experience a bit of anxiety about it, we stopped doing it!’ Just the same for any sort of anxiety, the best way to manage it is to face it head-on with the right tools and with a positive outcome [my parent left, I went to sleep on my own, I woke up and they were there again!] Mastering separation is an important life skill, and sleep times are a great way to practice this in a safe, controlled environment. You are building life skills by staying consistent and setting boundaries. Boundaries are the highest form of love!
That about sums up the 1-year-old crowd! Please come back to find age 2, 3, and 4 – coming soon!
Pam Edwards is a Certified Infant & Child Sleep Consultant and founder of Wee Bee Dreaming Pediatric Sleep Consulting, based out of Kamloops, B.C. Healthy sleep is addicting and she has made it her life mission to help families all across the world get the sleep they deserve - a good night's sleep doesn't have to be a dream!








![BACK TO SCHOOL! 📚 🍎
While there is a lot of uncertainty in our house with school this year [as I'm sure most families are experiencing!] one thing for certain is that we've got to scale back our ☀️summer bedtimes☀️ for back to school next week!](https://images.squarespace-cdn.com/content/v1/52531afee4b0f4b1f8aa79be/1601470556866-QORB0LBNG8Q204V7Y50N/image-asset.jpeg)
![CONTEST CLOSED⭐️GIVEAWAY/REVIEW!⭐️
I may have found my new favorite sound machine - introducing the SNOOZ!
Why do I ❤️love❤️ it so much?
🎵Lately I've been a big fan of pure #whitenoise [i.e. not an audio track] and the @snooz has a re](https://images.squarespace-cdn.com/content/v1/52531afee4b0f4b1f8aa79be/1601507619148-KSB6PM01DMX88BN903PG/image-asset.jpeg)
![DREAMFEEDING! 🌙 🍼
I've never done a DF with any of my kids [mainly because as babies I felt I worked so hard to get them to sleep, I'd be darned if I was going to risk waking them up!] but I've seen it work amazingly well for families I'm worki](https://images.squarespace-cdn.com/content/v1/52531afee4b0f4b1f8aa79be/1601507619148-1CJQR7LI3HD59XAKDBJK/image-asset.jpeg)