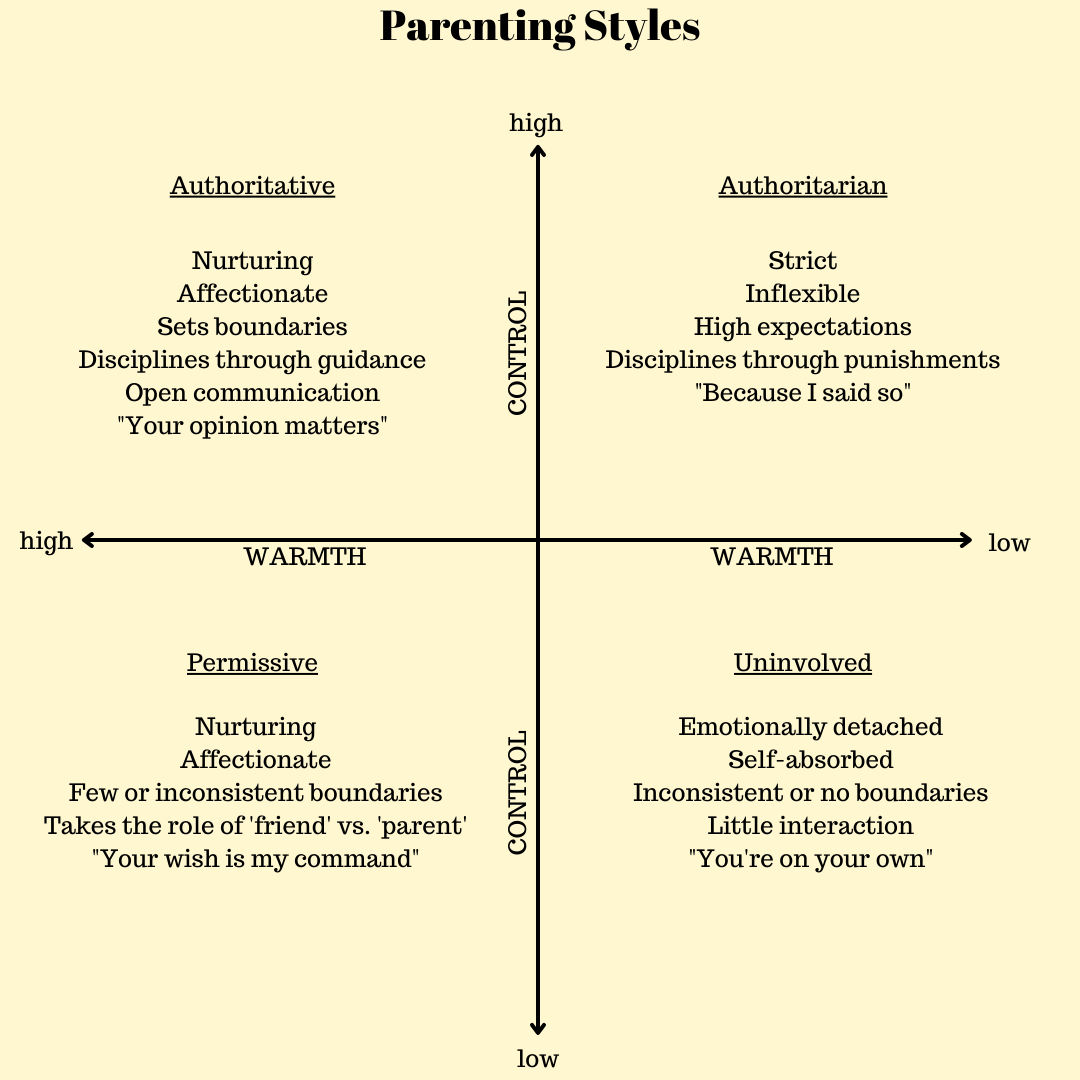
Gentle parenting, conscious parenting, respectful parenting – it has a lot of names. This parenting method is evidence-backed and shown to help raise children that are confident, independent, and happy. You may have heard of the term ‘Authoritative’ parenting which is what this parenting style strives to encompass. You are your child’s coach and you are aiming to cultivate a relationship where your child feels safe, comfortable, and able to express themselves without judgement, correction, or reprimand. It is not to be confused with a ‘Permissive’ parenting style where children have very few/no boundaries and parents are more of a ‘friend’ than a parent figure or ‘Attachment’ parenting which has a more rigid set of principles surrounding being always physically close to your child [breastfeeding, bedsharing, and baby wearing, as examples].
Gentle parenting is based on 4 main tenants, and below I will describe each and how I feel these can be related to the sleep training/independent sleep process:
Empathy
When it comes to having an empathic response to your child, this means we are trying to understand how your child is feeling in their moment. We do this by being mindful of our own response and exuding calm and confidence when responding to big feelings. Having a clear and predictable response helps us to feel less tense and anxious when responding to any protesting/crying at sleep times. Understanding that many of these big feelings are simply fatigue [not all, but many!] and by encouraging sleep, you are effectively meeting that need. “A gentle parent will not impulsively try to stop a frustrated child from crying. Instead, they’ll remain calm to show the child they can safely experience their negative emotions. They might honor the child's experience by telling them, "I can see you have strong feelings right now. Let's sit here together and take some deep breaths.” When parents don't immediately try to eliminate their child’s negative feelings, children feel accepted and learn to recognize the full spectrum of emotions as natural. They also learn to manage them in a peaceful and nurturing environment, building resilience against a flood of what would otherwise be deemed “negative” emotions.” (source: A Beginner’s Guide to Gentle Parenting)
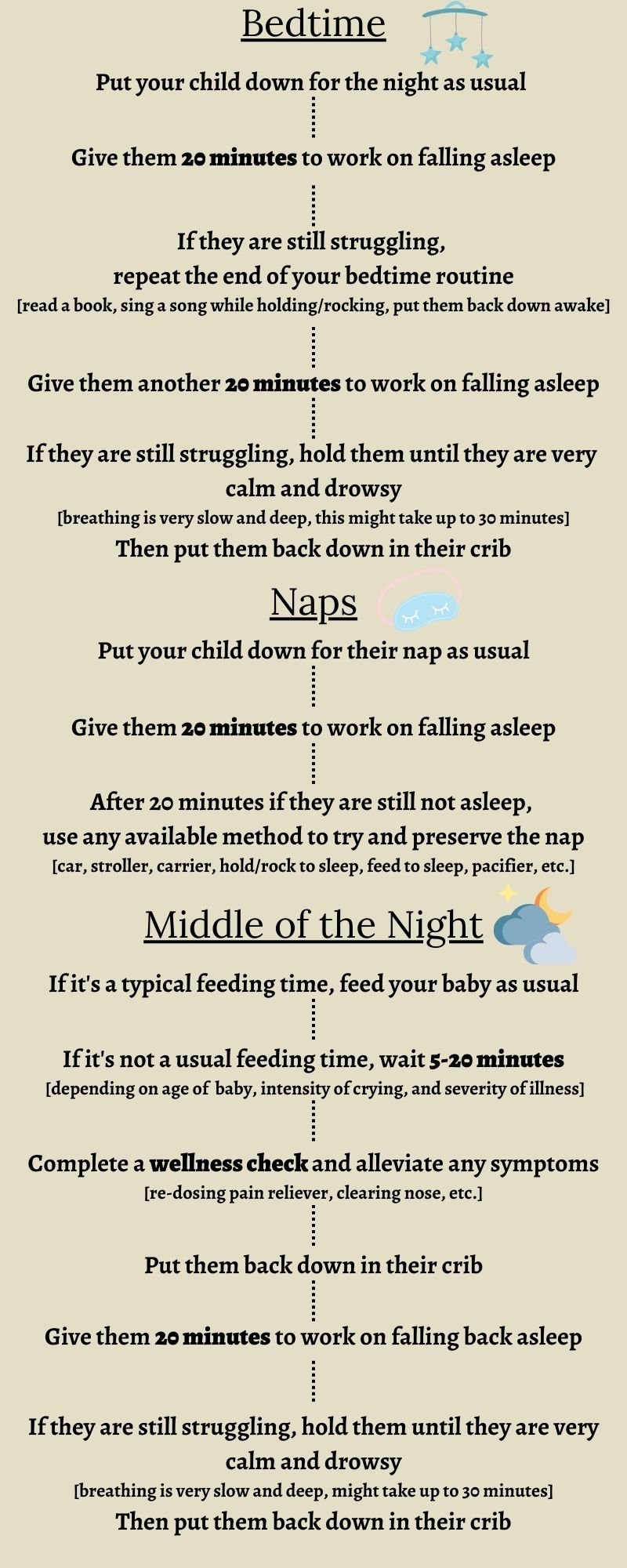
Sleep training gets a bad reputation from stories of simply laying your child down, shutting the door, and not coming back until the morning. It’s possible to sleep train with empathy – we can be there with your child while they work on this new skill, whether it’s by staying in the room or frequently reassuring your child along the way. Gentle parenting isn’t meant to eliminate any obstacles for your child along the way [aka bulldozer parenting], it’s giving them space to feel their feelings and letting them know that those feelings are safe with us, no matter how big or small. We want them to know that no matter how big those emotions get, they don’t scare us. That even when it’s hard, we know they can do it, and that you’ll be there with them to help in the process. This is exactly what sleep training is – believing in your child’s ability to learn a skill that can be difficult and frustrating at first, but will be beneficial for them for the rest of their lives, and coaching them through the process!
Respect
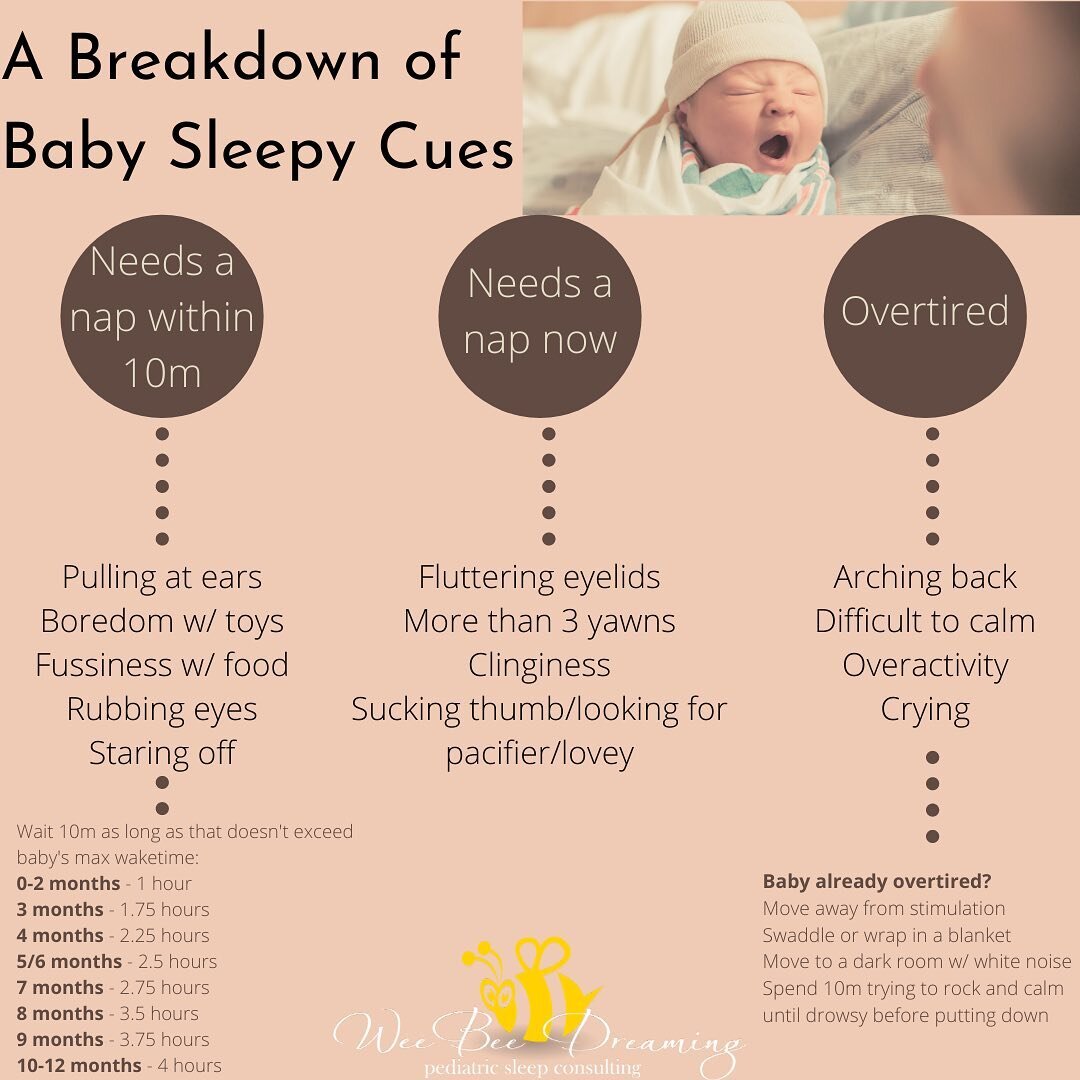
Gentle parenting is built on the premise of mutual respect, and the concept is simple – if you show your child respect, they will likely grow into an adult that respects others as well. A big bonus of sleep training is that it helps to respect our child’s need for sleep. Babies and toddlers are rarely convenient when it comes to sleep needs, especially young babies who need a LOT of sleep. By being mindful of this, we are respecting their need for rest to help their growing brains and bodies. Sometimes this means making difficult choices for their benefit – whether that means skipping events that will cause overtiredness or undergoing a sleep training endeavour if your child is not sleeping well. Respectful sleep training might also mean not being too hyper-fixated on getting your baby to sleep a certain number of hours or comparing them to your friend’s child that was sleep trained in one day, or a book that tells you that your child should be sleeping 12 hours every night – it means focusing on improving everybody’s well-being and remembering that your child is an individual with different needs, strengths, and weaknesses.
Understanding
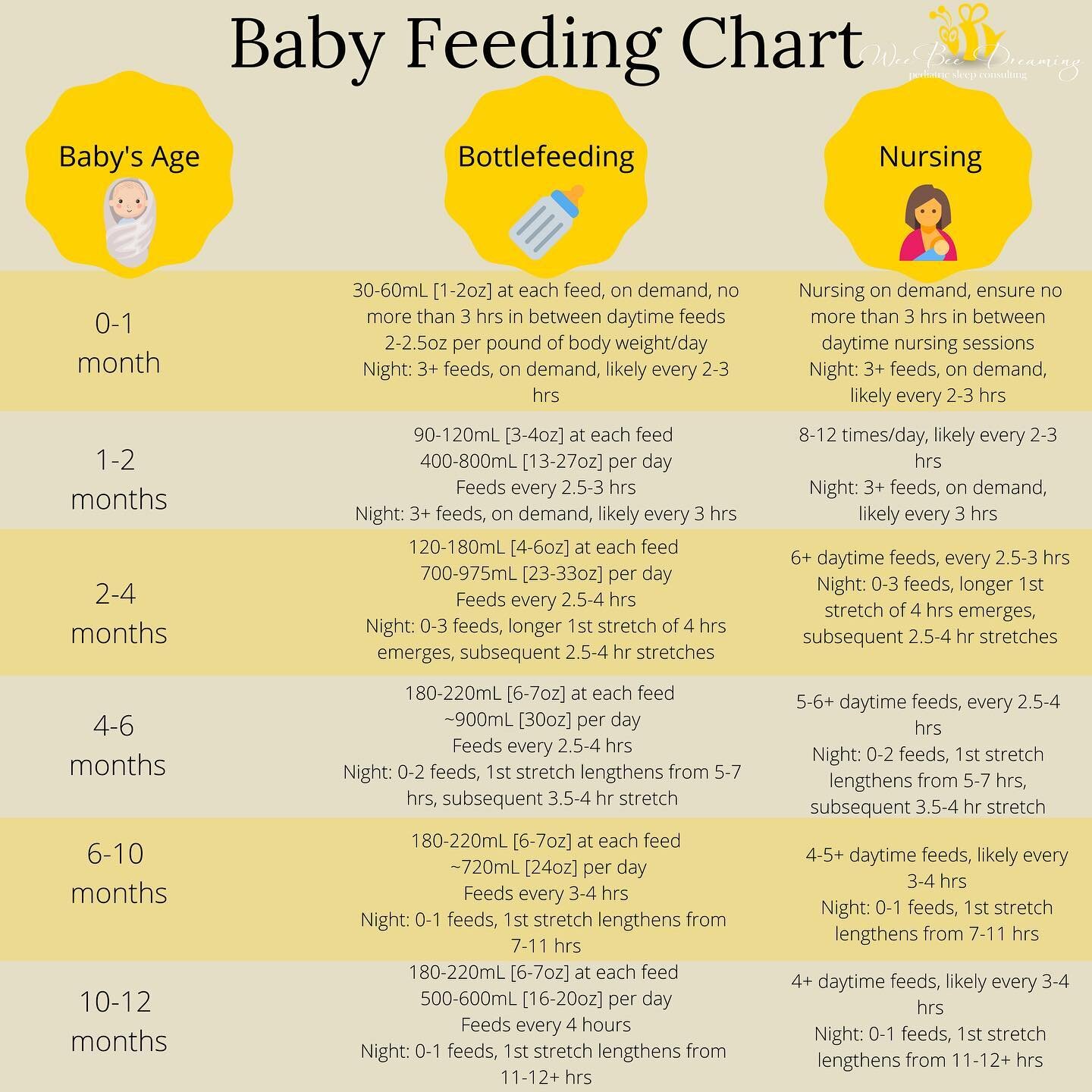
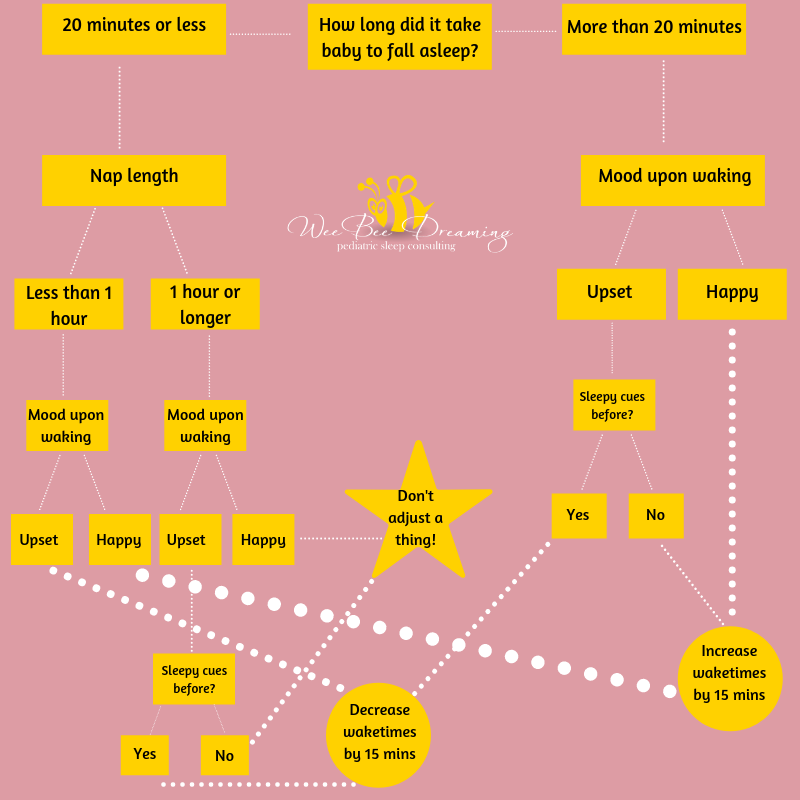
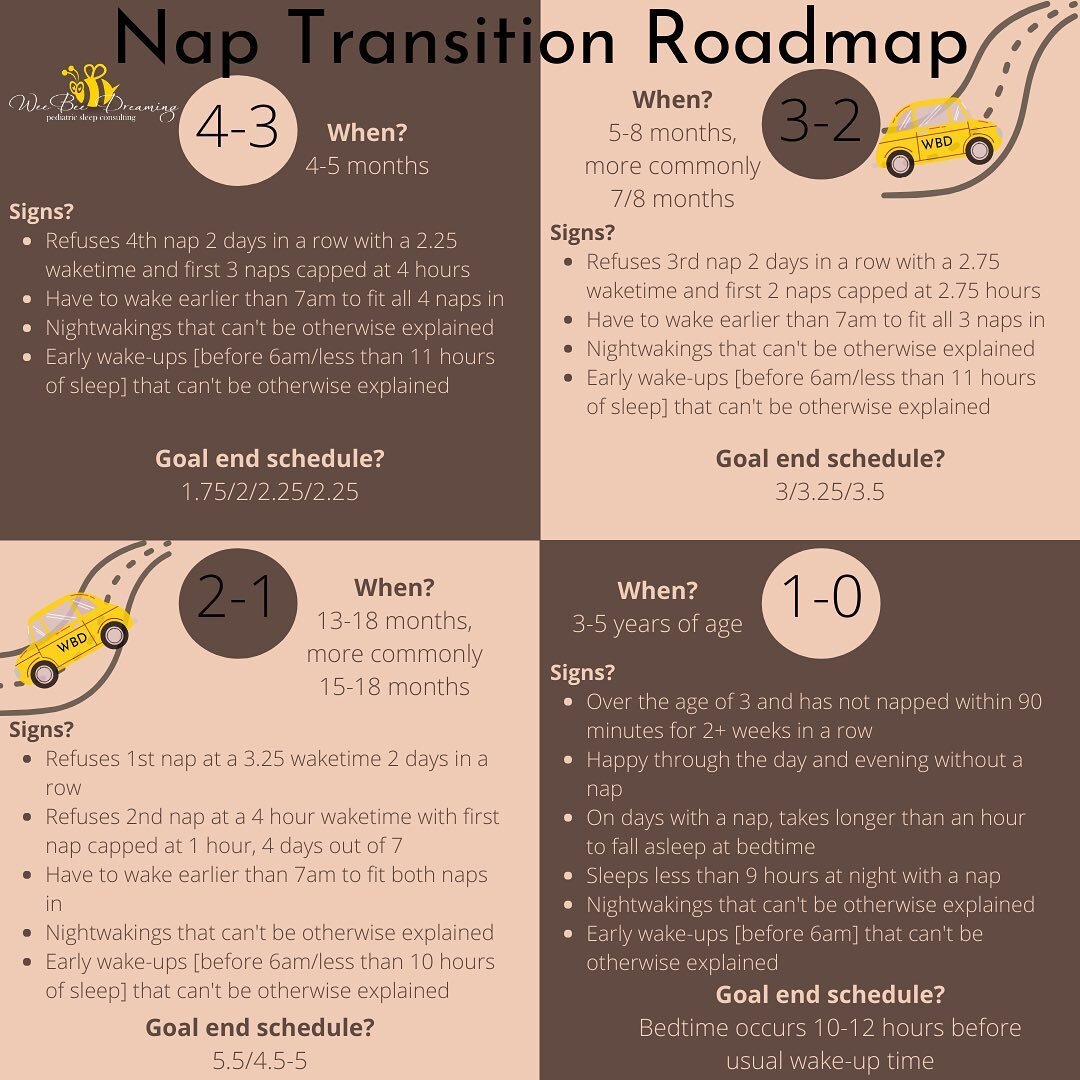
Part of sleep training is understanding what is realistic with your child’s sleep based on the age and stage they are in. Sleep training isn’t meant to fight against this, it’s meant to cultivate habits that set a child up to sleep the best they can at the age/stage they are in. Sleep training isn’t meant to push a child to sleep through the night before they are ready or to not express a need when a need is present, but it helps to separate the ‘needs’ from the ‘wants’ [i.e., I need to sleep, I need to eat, but I don’t need a parent to rock me to sleep and back to sleep 10 times each night]. In reality, we are all ‘sleep training’ whether we believe in the concept or not, traditional sleep training practices just assume we are sleep training to be independent in our sleep vs. sleep training to require a parent to help me sleep. A gentle parent can understand when the current routine is no longer working for a child and help them to learn a new and effective way of sleeping that will benefit the child and the entire family. But it is also important to understand that at different stages, sleep can be easier or more challenging, and it’s important to always remember that it is okay to deviate from your sleep plan to help your child through a tough phase – whether it be teething, illness, separation anxiety – you name it. Sleep training isn’t a ‘one way or the highway’ outlook – being flexible is always okay, just remember that getting back on track is important too!
Boundaries
This is probably the biggest concept that aligns with a sleep training philosophy – gentle parenting is based on setting clear and consistent boundaries for your child. The more consistent we are with our children [whether we’re talking sleep or not] the more your child will understand and respect your expectations for their behaviour. This could not ring any more true when it comes to expectations around sleep – we show our children through setting these expectations what we expect from them at sleep times. Whether the expectation is to require rocking or a feed to sleep, whether a pacifier will be replaced, whether we expect them to fall asleep on their own, and so on. Predictability is extremely comforting to children, and knowing what to expect at sleep times can be very reassuring.
This also means that when there are sleep issues present and your child is not getting the rest they so very need that it’s okay and important to set boundaries and make those necessary changes to help your child sleep. Boundary-setting is effectively just a set of family rules that you work to uphold. These can be things like having a set naptime each day, being consistent with what time bedtime is even if your child resists, being consistent in how your child goes to sleep, or having a consistent bedtime routine [again, even if your child resists!] Kids are going to push these boundaries, it’s part of their development. What kids are often craving is just for someone to acknowledge their feelings, ‘I know it’s hard, you are safe here, but it’s time to sleep now, and I’m going to turn off the light’. Babies of course cannot knowingly push boundaries but remember that a lot of the protesting we experience is due to you meeting a need that they didn’t yet know they had – you are changing their diaper before they are uncomfortable, you are feeding them before they are starving, and you are putting them down for sleep before they are exhausted. Always remember that emotions are not an emergency, and it gives children confidence and secure feelings of attachment to know that they have a caregiver looking out for their needs and who will always be a safe sounding board for feelings and emotions without any of those things being too overwhelming to bear. If every cry sends us into a tailspin and puts these boundaries on the backburner, it’s more difficult for your child to feel safe and secure. It leaves a child feeling even more anxious and leaves them without important lessons in being patient, understanding, and how to cope with disappointment.
While I never like to put too many labels on anything when it comes to parenting [gentle parenting, gentle sleep training, etc.] through my research on this parenting style, it has made me take a closer look into how I was raised and how I am raising my own children, and has been extremely eye-opening. I think that you absolutely can be a gentle parent and sleep train, as many of the principles overlap. I believe parenting without judgement of others is what we should all strive for, as we are all just doing the best we can with the resources we have available to us.
I want to especially thank all of you that have read my blog, engaged my services, or followed me on social media for letting me be a trusted resource in your parenting journey. If you are looking for support with your child’s sleep, please do not hesitate to reach out!
Pam Edwards is a Certified Infant & Child Sleep Consultant and founder of Wee Bee Dreaming Pediatric Sleep Consulting, based out of Kamloops, B.C. Healthy sleep is addicting and she has made it her life mission to help families all across the world get the sleep they deserve - a good night's sleep doesn't have to be a dream!






![BACK TO SCHOOL! 📚 🍎
While there is a lot of uncertainty in our house with school this year [as I'm sure most families are experiencing!] one thing for certain is that we've got to scale back our ☀️summer bedtimes☀️ for back to school next week!](https://images.squarespace-cdn.com/content/v1/52531afee4b0f4b1f8aa79be/1601470556866-QORB0LBNG8Q204V7Y50N/image-asset.jpeg)
![CONTEST CLOSED⭐️GIVEAWAY/REVIEW!⭐️
I may have found my new favorite sound machine - introducing the SNOOZ!
Why do I ❤️love❤️ it so much?
🎵Lately I've been a big fan of pure #whitenoise [i.e. not an audio track] and the @snooz has a re](https://images.squarespace-cdn.com/content/v1/52531afee4b0f4b1f8aa79be/1601507619148-KSB6PM01DMX88BN903PG/image-asset.jpeg)
![DREAMFEEDING! 🌙 🍼
I've never done a DF with any of my kids [mainly because as babies I felt I worked so hard to get them to sleep, I'd be darned if I was going to risk waking them up!] but I've seen it work amazingly well for families I'm worki](https://images.squarespace-cdn.com/content/v1/52531afee4b0f4b1f8aa79be/1601507619148-1CJQR7LI3HD59XAKDBJK/image-asset.jpeg)